Introduction:
Vertigo is a disorienting sensation of dizziness or spinning, often caused by issues in the inner ear or the brain. Benign Paroxysmal Positional Vertigo (BPPV) is one of the most common forms of vertigo, leading to sudden and intense bouts of dizziness triggered by specific head movements. These conditions can be debilitating and affect daily life. In this article, we will delve into the causes, symptoms, and treatment options for vertigo and BPPV, exploring how Solace Physio can offer effective relief and support for those experiencing these challenges.
Section 1: What is Vertigo and BPPV?
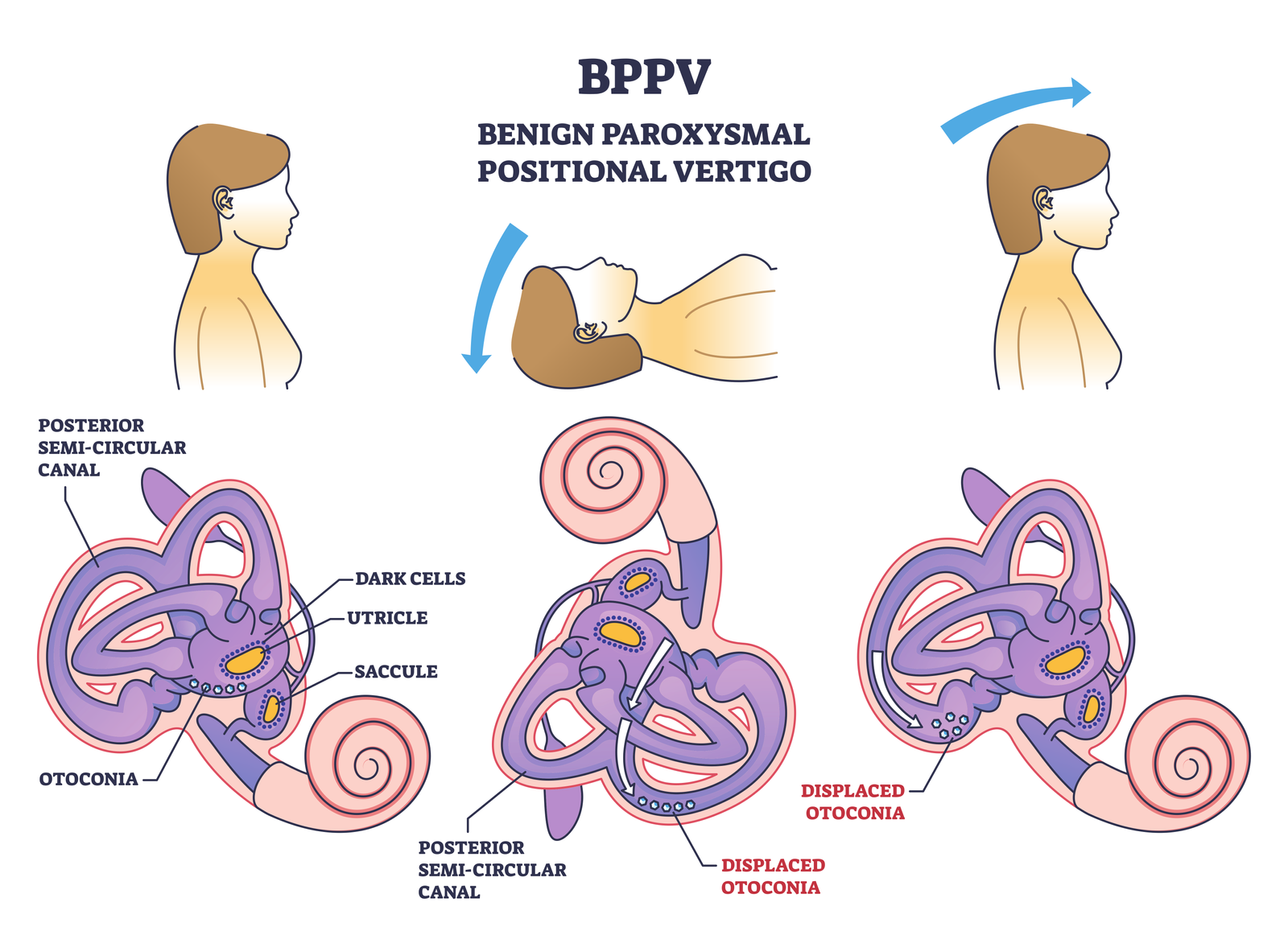
Vertigo is a false sensation of movement that makes individuals feel as though their surroundings are spinning or moving even when they are stationary. BPPV is a specific type of vertigo triggered by changes in head position, such as turning over in bed or looking up. It occurs when tiny calcium crystals in the inner ear, known as canaliths, become dislodged and stimulate the sensitive balance receptors.
Section 2: Causes and Risk Factors
Vertigo can result from various underlying conditions, such as inner ear disorders, vestibular migraines, Meniere’s disease, and vestibular neuritis. BPPV, on the other hand, is commonly caused by head injuries, aging, or changes in ear anatomy. Certain risk factors, such as a history of ear infections, head trauma, or a family history of vertigo, may increase the likelihood of developing these conditions.
Section 3: Recognizing the Symptoms
The symptoms of vertigo and BPPV can be distressing and often include:
- A spinning sensation
- Loss of balance or unsteadiness
- Nausea and vomiting
- Blurred vision
- Sweating
It is essential to differentiate vertigo from other forms of dizziness, as accurate diagnosis is crucial for effective treatment.
Section 4: Diagnosis and Treatment
At Solace Physio, we specialize in diagnosing and treating vertigo and BPPV. Our skilled physiotherapists conduct comprehensive assessments, including a thorough medical history review and physical examination. We may also use specialized tests, such as the Dix-Hallpike maneuver, to confirm BPPV.
For BPPV, a common treatment known as the Epley maneuver is often used to reposition the displaced crystals and alleviate symptoms. Additionally, our expert physiotherapists may recommend specific vestibular rehabilitation exercises to improve balance, reduce dizziness, and enhance the brain’s ability to compensate for inner ear imbalances.
Section 5: Vestibular Rehabilitation at Solace Physio
Solace Physio offers tailored vestibular rehabilitation programs to address vertigo and BPPV. Our approach aims to restore the body’s natural balance and minimize symptoms. Through a combination of hands-on techniques, exercises, and lifestyle modifications, we help patients regain control over their balance and improve their overall quality of life.
Section 6: Preventive Measures and Lifestyle Tips
To reduce the risk of vertigo and BPPV episodes, Solace Physio provides essential preventive measures and lifestyle tips. These may include:
- Maintaining good posture
- Taking care when changing head positions
- Avoiding sudden movements
- Managing stress and anxiety levels
Conclusion:
Vertigo and BPPV can be disruptive to daily life, but with the right diagnosis and treatment from Solace Physio, relief is within reach. Our experienced physiotherapists are well-equipped to address the underlying causes of vertigo and BPPV, providing personalized vestibular rehabilitation programs to help patients regain their balance and confidence. Don’t let vertigo control your life; take the first step towards relief and reclaim your equilibrium with Solace Physio’s specialized care.