Introduction:
Urinary incontinence and pelvic floor dysfunction are two common conditions that can significantly impact a person’s quality of life. These conditions are often interlinked and can affect individuals of all ages and genders. In this article, we will explore the causes, symptoms, and treatment options for urinary incontinence and pelvic floor dysfunction, shedding light on how Solace Physio can provide relief and support to those experiencing these challenges.
Section 1: Understanding Urinary Incontinence
Urinary incontinence refers to the involuntary leakage of urine. It can occur due to various reasons, including weakened pelvic floor muscles, hormonal changes, urinary tract infections, neurological disorders, and lifestyle factors. There are different types of urinary incontinence, including stress incontinence, urge incontinence, overflow incontinence, functional incontinence, and mixed incontinence.
Section 2: Pelvic Floor Dysfunction Explained
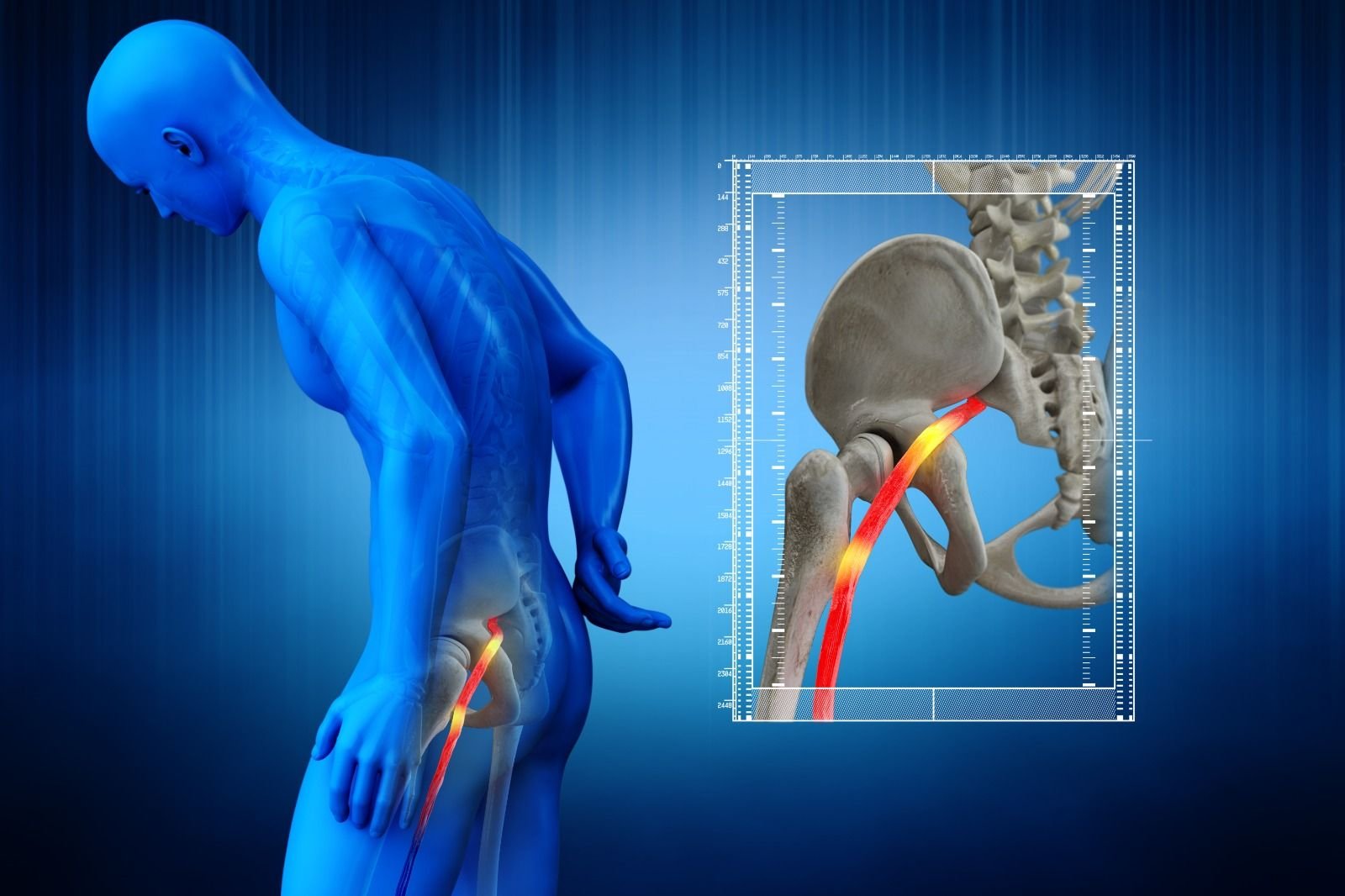
Pelvic floor dysfunction refers to a condition where the muscles, ligaments, and connective tissues in the pelvic floor become loose, dysfunctional. This dysfunction can lead to a range of symptoms, including urinary incontinence, fecal incontinence, pelvic pain, sexual dysfunction, and organ prolapse. Factors contributing to pelvic floor dysfunction include pregnancy and childbirth, hormonal changes, obesity, chronic constipation, and certain medical conditions.
Section 3: Symptoms and Diagnosis
Recognizing the symptoms of urinary incontinence and pelvic floor dysfunction is crucial for seeking appropriate treatment. Symptoms of urinary incontinence include frequent urination, urgency to urinate, leakage during physical activities or sneezing, and nocturia (waking up multiple times during the night to urinate). For pelvic floor dysfunction, symptoms may include pelvic pain, discomfort during intercourse, bowel movement difficulties, and a sensation of heaviness in the pelvic region.
Accurate diagnosis is essential, and healthcare professionals, such as those at Solace Physio, can conduct a thorough assessment, including a physical examination, medical history review.
Section 4: Treatment Options
Fortunately, both urinary incontinence and pelvic floor dysfunction are treatable conditions. Solace Physio offers a variety of evidence-based treatments tailored to each individual’s specific needs. These treatment options may include:
- Pelvic Floor Muscle Exercises: Strengthening the pelvic floor muscles through targeted exercises can significantly improve bladder control and alleviate symptoms.
- Biofeedback: This technique helps individuals learn how to control and strengthen their pelvic floor muscles by providing visual or auditory feedback on muscle activity.
- Lifestyle Modifications: Solace Physio can provide guidance on lifestyle changes such as managing fluid intake, dietary adjustments, and establishing healthy toilet habits to improve bladder and bowel control.
- Behavioral Therapy: This approach aims to identify and modify any behavioral patterns or habits that contribute to urinary incontinence or pelvic floor dysfunction.
Section 5: Maintaining Long-Term Pelvic Health
To maintain long-term pelvic health, Solace Physio emphasizes the importance of self-care practices and ongoing support. These may include regular exercise, incorporating relaxation techniques, practicing good posture, managing stress levels, and following personalized maintenance plans.
Section 6: Prevention and Self-Care Tips
While treatment options are available for urinary incontinence and pelvic floor dysfunction, incorporating preventive measures and self-care practices can also play a vital role in maintaining pelvic health. Here are some helpful tips:
- Maintain Healthy Weight: Excess weight can put added pressure on the pelvic floor muscles, contributing to dysfunction. Aim to maintain a healthy weight through a balanced diet and regular exercise.
- Stay Hydrated: While it may seem counterintuitive, drinking an adequate amount of water throughout the day is important for bladder health. Avoid excessive fluid intake close to bedtime to minimize nocturia.
- Avoid Straining During Bowel Movements: Straining during bowel movements can strain the pelvic floor muscles. Ensure a fiber-rich diet, stay hydrated, and establish regular bowel habits to prevent constipation and reduce the risk of pelvic floor dysfunction.
- Practice Good Posture: Maintaining good posture helps support the pelvic floor and reduces the risk of strain on the muscles. Sit and stand with your spine aligned and avoid prolonged periods of sitting or standing in the same position.
- Exercise Regularly: Engaging in regular physical activity helps improve overall muscle tone and strength, including the pelvic floor muscles. Incorporate exercises such as walking, swimming, yoga, and Pilates into your routine.
- Manage Chronic Cough: Frequent coughing can strain the pelvic floor muscles. If you have a chronic cough, seek medical attention to address the underlying cause and minimize its impact on your pelvic health.
- Practice Stress Management: Chronic stress can contribute to pelvic floor dysfunction. Explore stress-reducing techniques such as meditation, deep breathing exercises, and engaging in activities that bring you joy.
- Avoid Smoking: Smoking can impair the blood flow to the pelvic region, leading to compromised pelvic floor function. Quitting smoking can significantly improve overall pelvic health.
Section 7: Seeking Professional Help at Solace Physio
If you are experiencing symptoms of urinary incontinence or pelvic floor dysfunction, it is essential to seek professional help from experienced physiotherapists specialized in pelvic health, such as those at Solace Physio. They can provide an accurate diagnosis, develop personalized treatment plans, and guide you through the rehabilitation process.
Solace Physio takes a holistic approach, considering not only the physical aspect but also the emotional and psychological well-being of their patients. They create a supportive and comfortable environment where individuals can openly discuss their concerns and receive personalized care.
Remember, you are not alone in your journey toward pelvic health. With the guidance of Solace Physio’s experts and your commitment to self-care, you can overcome the challenges of urinary incontinence and pelvic floor dysfunction, reclaiming a life of confidence, comfort, and freedom.
Conclusion:
Urinary incontinence and pelvic floor dysfunction can significantly impact one’s daily life and overall well-being. However, with the right guidance, support, and evidence-based treatments from Solace Physio, individuals can regain control over their pelvic health. By understanding the causes, recognizing the symptoms, and exploring the available treatment options, individuals can take proactive steps towards a life free from the limitations and discomfort associated with these conditions.