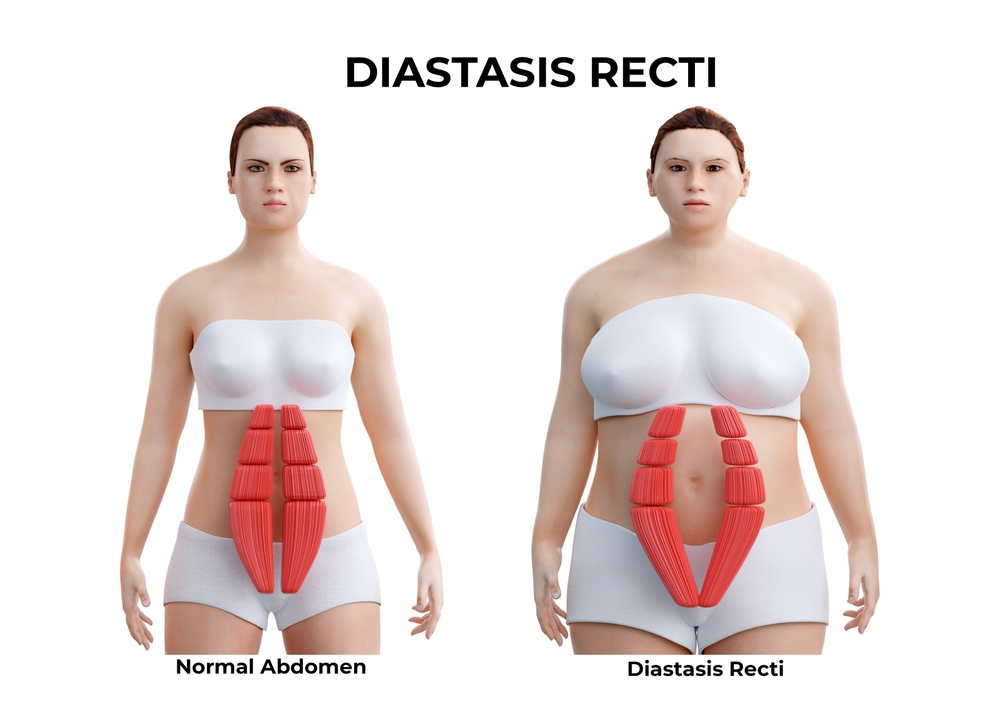
During pregnancy, a woman experiences several changes in her body- From weight gain to hormonal and abdominal changes. One such condition post-child-berth is known as Diastasis abdominal rectus. This condition occurs when left and right abdominous tissue stretches and separates. While this is a natural occurrence during pregnancy, the persistence of it can affect core strength and appearance.
Understanding Diastasis abdominal rectus
Diastasis abdominal rectus, also known as Diastasis recti is an increased gap between rectus abdominis muscles. This condition can erupt during pregnancy due to a lack of abdominal strength. It can cause pain in the back, poor body posture, and visible bulges in the abdomen.
Importance of Physiotherapy in Recovery
Physiotherapy plays a crucial role in the recovery from Diastasis recti after childbirth. Seeking physiotherapy to cure Diastasis recti can help reduce the recovery time, ease pain, and reduce discomfort. Physiotherapy focuses on targeted muscle exercise to reduce the gap between separated muscles and strengthen the lower pelvic core.
Recovery after Childbirth
Recovery from childbirth is generally a slow and gradual process. It takes time to recover and understandably so. A Woman body’s goes through a lot of changes in the pre-natal stage. So to recover from this requires a lot of discipline and dedication. Physiotherapy aids in this overall process and if followed with the right plan, makes the recovery quicker and more healthier.
Under the guidance of a physiotherapist
Seeking the help of a physiotherapist in recovery helps reduce the pain and shorten the time duration of recovery. Here’s how it can help.
- Regular assessment and customized treatment: A physiotherapist assesses the severity of the problems before coming up with a customized treatment plan. They tailor plans based on individual needs and body.
- Targeted exercise: A physiotherapist prescribes the targeted exercise to strengthen the core muscle. When having conditions such as abdominus rectus, supervised exercise is a must because it can turn to worse.
- Education: Besides exercise, a physiotherapy session educates women about health, posture correction, and post-natal recovery. This guidance helps prevent further strain on weakened abdominal muscles.
Recovery with SolacePhysio
Solace Physiotherapy has been a standout clinic in North Vancouver, Canada, providing all the physiotherapy services, including pre and post-natal therapy sessions to treat Diastasis abdominus rectus.
We have a team of physiotherapists dedicated to helping women recover from this condition. Our holistic development approach is coupled with modern facilities and technologies to help women regain confidence post-pregnancy.
Through targeted exercise and one-on-one sessions with our physiotherapists, we support women in restoring optimal pelvic floor function. So, if you reside nearby, do give us a call or visit our website. We will be happy to be part of your transformative journey.
Conclusion
Diastasis abdominis rectus is a condition while challenging, can be effectively managed and treated with the right approach. This is a common postpartum condition that requires focused attention and proper care for effective recovery. With the expertise and support of clinics like Solace Physio in North Vancouver, women can confidently embark on the path to reclaiming their physical well-being post-childbirth. Remember, recovery is a journey, and with the right guidance and support, every step forward brings you closer to a stronger, healthier you.